Following a low FODMAP diet? Here’s our advice on getting a healthy balance.
The first stage of a low FODMAP diet (known as elimination) involves swapping high FODMAP foods for low FODMAP alternatives for a period of 2-6 weeks, to see if IBS symptoms improve.
As with any diet which restricts certain foods, there is a risk of not getting enough of some nutrients during the elimination phase. Here’s our advice on maintaining a healthy balance whilst following a low FODMAP diet.
Tips to Eating Healthily Whilst Following a Low FODMAP Diet
1. What You Remove, Replace
The key to keeping a healthy balance of all the important nutrients in your diet during elimination is to make sure that whatever high FODMAP food you remove, you replace it with a low FODMAP alternative that contains similar nutrients.
This might sound complicated – but think in terms of like for like. For example, if you currently eat weetabix for breakfast, you could replace it with oats. And instead of regular milk you could choose lactose free milk. If you usually eat an apple as a snack, replace it with a bunch of grapes. And so on.
2. Take Care With Calcium & Fibre
Two nutrients which deserve special attention when following the low FODMAP diet are fibre and calcium. Fibre is found in carbohydrate foods like cereal grains, fruits, vegetables, beans, peas and lentils, nuts and seeds – all foods which are restricted to some degree during elimination. If you struggle with constipation, try to choose higher fibre options .
Tips for increasing fibre without FODMAPs
- Choose oats for breakfast. A serving is half a cup (50g)
- Snack on low FODMAP fruit or add to breakfast; bananas, raspberries, rhubarb, kiwifruit, oranges, strawberries, blueberries, pineapple, passion fruit and oranges
- Include 2 portions of low FODMAP vegetables with your meals; carrot (skin on), green beans, potato (skin on), spinach, courgettes, aubergine, peppers are all low FODMAP
- Check food labels when buying low FODMAP bread and cereal products. Compare the ‘per 100g’ column to find higher fibre options. A high fibre option will contain 6 grams or more of fibre per 100 grams. Examples include quinoa, brown rice, gluten-free multigrain bread, rice bran, oat-bran, and porridge (oats).
Most of the calcium in our diets comes from dairy foods. Because regular cow’s milk and yoghurt are restricted on the elimination phase, calcium intakes can be low too. Choose a lactose-free cow’s milk or choose a calcium-fortified plant milk to meet your calcium needs, and try to eat 2-3 portions of dairy foods a day. An example would be a serving of milk on cereal, a pot of lactose-free yoghurt and a portion of cheese – many firm kinds of cheese (including brie, cheddar and comte) are low FODMAP.
3. Get Your 5 A Day
Fruit and vegetables are a major source of vitamins and minerals, but also plant fibres that help to feed the beneficial microbes living in your gut. This makes them a really important part of a healthy diet. In the UK it’s recommended we aim for 5 portions a day – a portion being equal to around 80 grams.
What is 80 grams? It’s equivalent to a medium sized fruit like a banana or orange, two small fruits (like kiwis), three heaped tablespoons of cooked vegetables, or a bowl of salad leaves.
Although there are a large number of fruits and vegetables which are high in FODMAPs and not suitable during elimination, there are also plenty which are low FODMAP.
Some of our favourites include aubergines, peppers, rocket, olives, spinach, cherry tomatoes, kiwis, strawberries, clementines, grapes, pineapple and oranges.
4. Have Healthy Snacks On Hand
Snacking can be a bit trickier on the FODMAP diet as typical snacks like biscuits and cereal bars tend to be high FODMAP. Choosing healthy snacks will help keep your energy levels steady, and (depending on what you choose!) can provide important nutrients including vitamins and fibre.
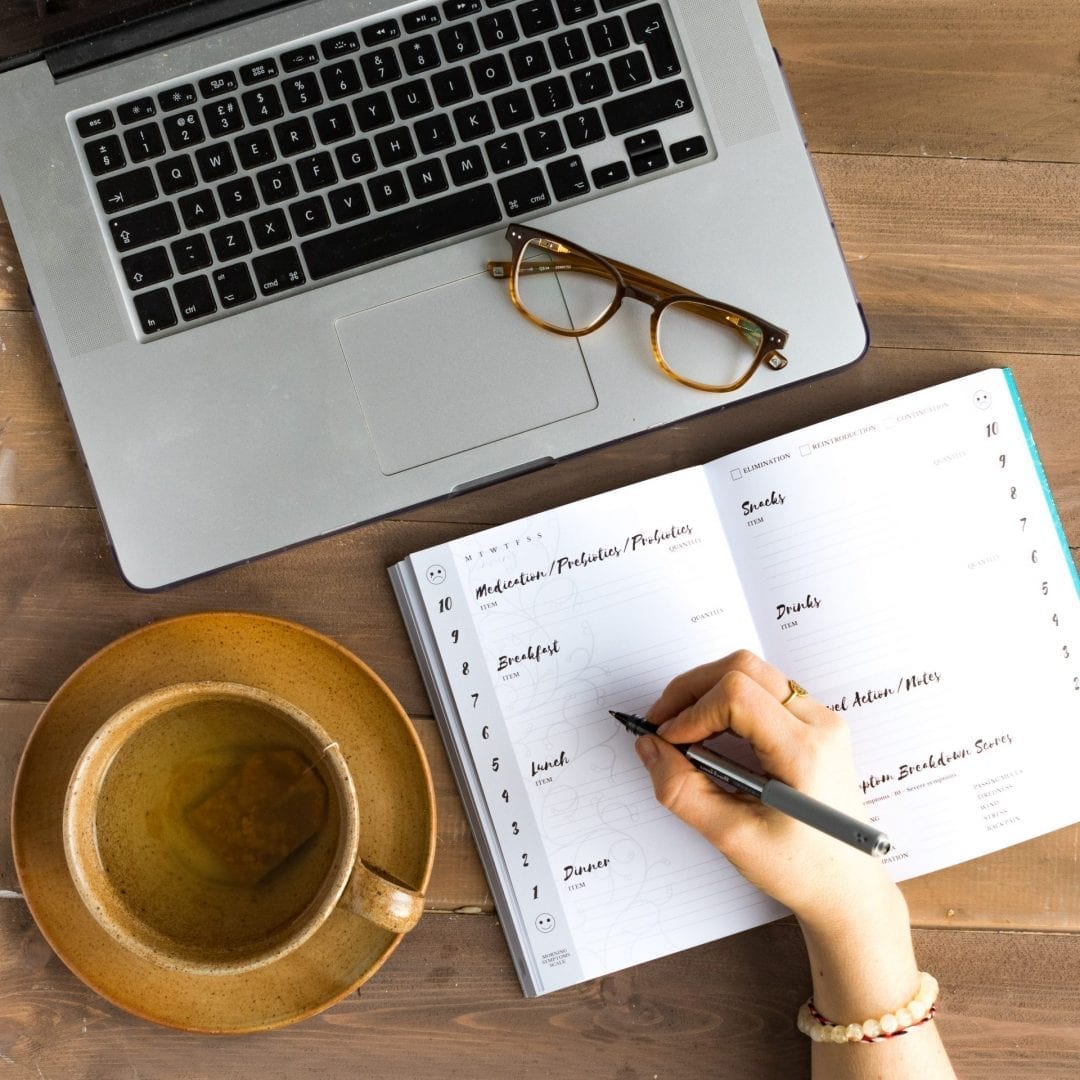
Try to keep some ready-to-eat FODMAP friendly snacks in your desk or bag so you have something to eat when hunger strikes.
Snack ideas
- Handful of walnuts
- Handful of grapes and cheddar slices
- Banana slices with spoonful of almond butter or peanut butter
- Oatcakes with nut butter
- Popcorn
- Dark chocolate (30g)
- Kiwi fruit or strawberries with lactose free yoghurt
5. Go Easy With Alcohol
Although many alcoholic drinks (like beer, wine and vodka) are low FODMAP, alcohol can still trigger symptoms. Studies show that about one third of people with IBS feel alcohol is a trigger, so it’s worth taking note of how alcohol affects your IBS.
The strongest links between alcohol and symptoms seem to be with heavy drinking – i.e. having several drinks in one go) and for those with diarrhoea predominant IBS.
If you notice a link, it’s worth cutting back. As a guide, if you are drinking, try to stick to a maximum of one drink in a sitting – for example a standard glass of wine, spirit and mixer or pint of beer.